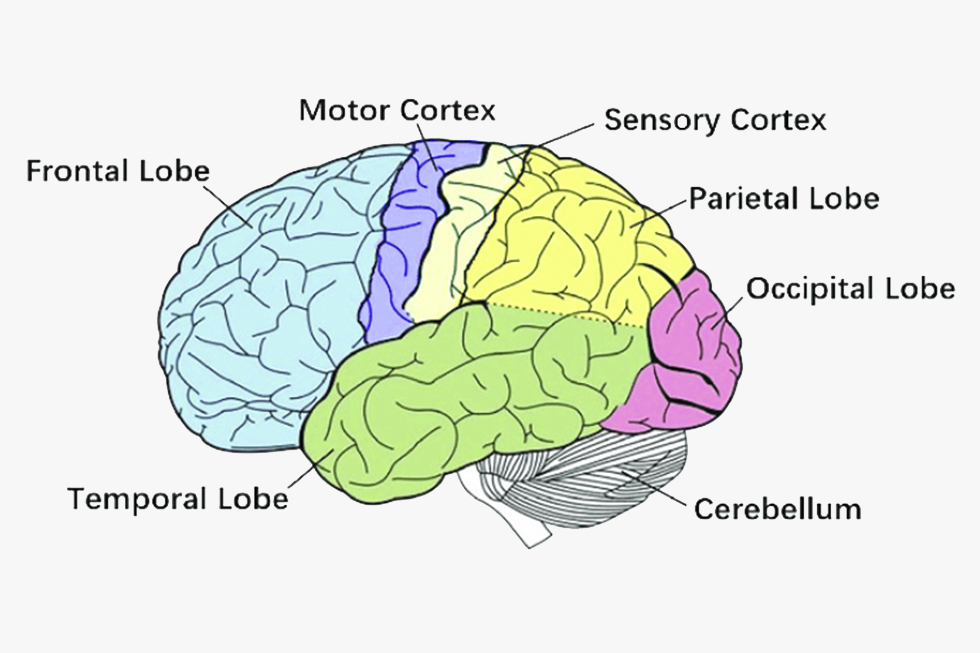
Parkinson’s Disease (PD) is a neurodegenerative disorder characterized by both progressive motor (physical) and nonmotor impairments. As nerve cells in the brain die, levels of the chemical dopamine decrease. Appropriate levels of dopamine within the motor and insular cortices are critical for maintaining normal movement and coordination, managing motivation, and reinforcing behaviors.
https://www.researchgate.net/figure/Primary-brain-regions-Motor-cortex-is-the-region-in-charge-of-planning-control-and_fig2_331905251
Motor symptom progression of PD includes:
- Gait dysfunction
- Tremor
- Impaired posture and balance
- Difficulty initiating + maintaining movement due to loss of automaticity
- Speech and swallowing deficits
- Slowed movements (bradykinesia)
Cognitive impairments are nonmotor disease progressions that further impact an individual’s safety and function. Cognitive functions frequently impacted include:
- Working memory
- Attention and time management
- Visuospatial function
- Executive function (planning, remembering instructions or items on a list)
- Cognitive reaction time
In addition, emotional changes (depression, anxiety), poor blood pressure regulation, fatigue, and pain may occur. As a result of both motor and nonmotor disease progression, PD leads to a decline in movement safety and increases an individual’s fall risk.
Medication Management
Physicians prescribe medication to help manage symptoms of PD. Dopamine itself cannot be directly given as it cannot cross into the brain. Levodopa is a natural chemical that is converted to dopamine. It is combined with carbidopa, termed carbidopa-levodopa, to prevent early conversion to dopamine prior to entering the brain. In addition, physicians may prescribe dopamine agonists which can copy the role of dopamine in the brain but are generally not as effective. Additional medications may also be utilized to manage symptoms of PD. The critical piece in relation to exercise and physical therapy intervention is to optimize medication timing to maximize participation and results within a scheduled time block.
Example of an everyday activity made more difficult by PD: Unloading groceries
Task requirements/sequence:
- Carrying bags from car into house/kitchen, may require car and house door management, walking up or down stairs, and safely navigating furniture
- Unpacking each bag and putting each object away in appropriate location, requiring movement combinations including squatting, lifting, side stepping/backwards stepping, and reaching high and low while safely holding objects of various weights
The physical energy, strength, and balance required to complete the task as well as utilizing proper task sequencing can cause increased fatigue and energy expenditure.
How can exercise help manage progression of PD symptoms?
Research has repeatedly shown consistent participation in cardiovascular and strength based training enhances functional performance through motor learning. Safe motor performance requires proper regulation of automatic (unconscious) and voluntary (cognitive) movement strategies. Some key takeaways from exercise based PD research include:
- Properly dosed aerobic exercise can increase production of dopamine (Matthew A. Sacheli et al 2019)
- Faster RPMs (higher intensity) while completing a cycling program improves motor outcomes/function (Angela L Ridgel et al 2009)
- Goal-based practice to improve a specific skill set, dynamic balance for example, requires feedback (reinforcement) to challenge patients, maintain motivation, and enhance cognitive awareness of previously automatic movements (Giselle M Petzinger et al 2013)
In general, exercise in PD has the potential to improve sleep, decrease fatigue, prevent depression, prevent cardiovascular disease complications, improve PD drug efficacy, and optimize dopamine production/use.
Exercise programs should be developed and monitored by a knowledgeable clinician who prioritizes management of motor and nonmotor impairments in an individualized manner. In addition, group exercise programs designed to improve balance, movement amplitude, strength, while developed to ultimately combine physical and cognitive tasks (dual-tasking) have the added benefit of socialization.
Reach out to us at Pursuit Physical Therapy to schedule your one-on-one evaluation and treatment programming with our Board-Certified Neurologic Clinical Specialist, Kaitlyn Malaski, PT, DPT, NCS.

