Do you have neck pain or stiffness?
Do you experience frequent headaches? Is it hard to rotate your head to look left or right when driving? Do you have to use pillows to prop up your head when sleeping? Do you find yourself looking down at the ground when walking?
If you answered yes to one or more of these questions, there are additional questions that a physical therapist should ask when evaluating you. There is often an association between neck pain, stiffness, and dizziness. Frequently, dizziness and its related symptoms are not seen as connected to the neck symptoms, but they need to be assessed this way! The following are just a sample of potential questions to determine if your neck pain/stiffness and other symptoms are potentially linked or impacting one another:
- Have you fallen or experienced unsteadiness?
- Is it harder for you to walk around in the dark?
- Do fast head movements in any direction make you feel disoriented?
- Does your head ever feel disconnected from the rest of your body?
- Do you ever feel lightheaded or faint, either when switching positions (moving from sitting to standing for example) or when you are walking around?
- Is the room ever spinning, particularly after rolling over in bed or looking up?
- Do you experience motion sickness OR have onset of dizziness in the days after traveling by plane or boat?
Why and how are these symptoms potentially linked?
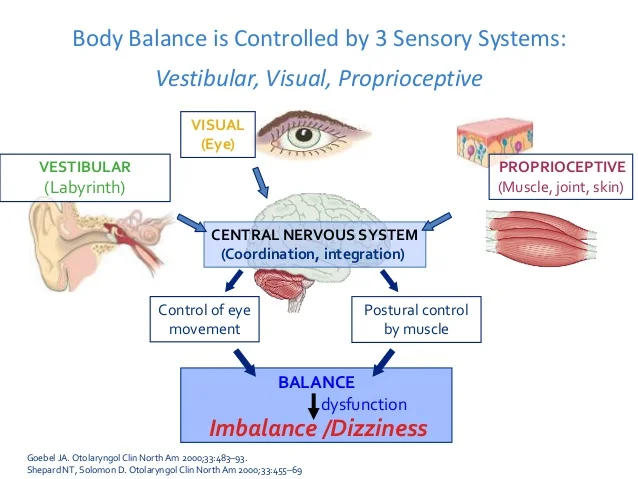
There are a few key points to understand here. Generally speaking, our sense of equilibrium is managed by sensory information (proprioception) from the muscles, joints, and skin throughout our body including our neck region (cervical spine). This information works together with visual (eye) and vestibular (inner ear) information to help us maintain our balance and move around without feeling “off”.
Now imagine a patient comes to a physical therapy evaluation reporting neck pain and stiffness. Below are several scenarios which are frequently observed or reported in the clinical setting.
(1) Scenario One: Patient reports they are having a hard time turning their head when driving because of pain. As this patient walks around the clinic, they are unable to separate head rotation from trunk rotation. They must turn their entire body to look left or right. This stiffness reduces the amount of isolated head rotation performed daily. Because the vestibular system is activated through repeated changes in head position, this loss in range of motion into rotation limits the amount of stimulation to the vestibular system. Now anytime this individual unexpectedly turns their head more than usual, the brain sends signals about dizziness being present.
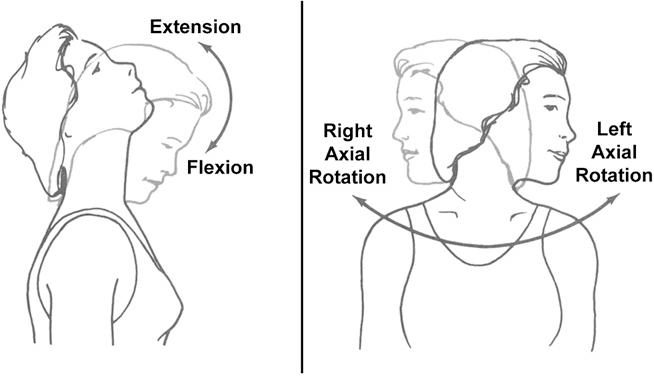
(2) Scenario Two: A patient has a hard time laying flat on their back in bed and must prop their head up using pillows. Movement into neck extension to look up into a high kitchen cabinet or store shelf is also painful. This prompted her to seek physical therapy services. Upon evaluation, it is revealed that when trying to wash her hair in the shower, she experiences brief periods of dizziness. Because the patient has limited movement when attempting to bring her head up/back, tasks that require this movement including washing her hair are more likely to cause dizziness. As was the case in the first scenario described, decreased frequency of movement into extension and the general loss of extension limits the amount of expected stimulation to the vestibular system.
These two scenarios are just two examples of how neck pain can feed into onset of dizziness with head movement. Like any part of the body, the vestibular system requires movement to stimulate the system and maintain its “fitness”. Lack of vestibular system fitness increases the likelihood that an individual will experience dizziness or any related symptoms (lightheadedness, “floatiness”, spinning, feeling like a bobblehead). This is critical to daily function because without the ability to successfully use vestibular information, people are at an increased risk for falls, deconditioning, and decreased independence. This often leads to an increased rate of injury and hospitalization.
It is important to note that not all dizziness is related to neck pain and/or stiffness. Dizziness is often multifactorial and requires a skilled clinician to determine the cause as well as an appropriate treatment plan. A history of concussion, whiplash, frequent ear infections, and migraines also contribute to presence of dizziness, even YEARS after initial injury such as concussion. A recent viral infection, including but not limited to Covid-19 can also lead to dizziness. In addition, a medical history that includes anxiety, depression, or PTSD has been found to contribute to increased risk for chronic dizziness.
If you or someone you know is experiencing dizziness or any related symptoms, whether acutely or chronically, call us at Pursuit Physical Therapy to schedule an individualized evaluation. This can be successfully treated through physical therapy intervention and without reliance on medication such as Antivert (Meclizine).